
Family Balancing & Laboratory
Family Balancing
We are one of the few clinics in St. Louis offering family balancing — or sex selection — on embryos, giving couples the capability of choosing their child’s gender.
A commonly asked question Dr. Saji Jacob and our team at GoFertility receive from patients is: “Do we offer family balancing — or sex selection — on embryos?” When patients meet a set of criteria detailed by Dr. Jacob during their in-office appointment, we do offer them the service of sex selection.
In family balancing, couples have the capability of choosing whether to have a boy or girl prior to becoming pregnant. Couples undergoing in-vitro fertilization (IVF) at GoFertility have the option of screening embryos and only transferring ones of the preferred sex into the uterus. Patients usually choose sex selection for one of two reasons:
1. They already have children of a certain gender — such as three boys — and want to ensure their next child is of the opposite gender to balance out their family. Sometimes couples wouldn’t have another child unless they knew with certainty the gender of that next child. Family balancing provides that capability.
2. One of the parents may be a genetic carrier for a specific sex-linked disorder — hemophilia, Duchenne muscular dystrophy or Fragile X syndrome, for example. If their baby was a male, that child would likely receive the disorder and have symptoms related to the disorder. A female baby, meanwhile, would likely simply be a carrier of the disorder and not have any disorder-related symptoms.
How does family balancing work?
While many St. Louis-area fertility clinics don’t offer family balancing or sex selection of embryos, GoFertility provides this service for couples who want it as part of the IVF treatment process. Recent advancements in technology have likewise caused a spike in the demand for gender selection.
Sex selection is completed with pre-implantation genetic testing-aneuploidy (PGT-A), a cutting-edge technology that tests the chromosomal composition of embryos. A mother’s eggs carry an X chromosome, while a father’s sperm carries either an X or Y chromosome. If an X chromosome from the father fertilizes the egg, a female embryo (XX) results. A Y chromosome fertilizing the egg results in a male embryo (XY).
Dr. Jacob — a trained embryologist, infertility specialist and board-certified as a high-complexity clinical lab director — and our clinical team screen each embryo using state-of-the-art equipment. Dr. Jacob and his staff can genetically determine whether an embryo is male or female and screen all 23 sets of chromosomes for abnormalities. This increases the chances of a healthy baby. A healthy embryo of the parents’ desired gender is then transferred to the patient’s uterus.
Any remaining chromosomally normal, or euploid, embryos can be stored for future use. If you think family balancing may be right for you, get in touch with CRMRS at 314-473-1285 or AGraham@GoFertility.com. We are always welcoming new patients into our Creve Coeur-located facility and can typically book appointments for you to meet with Dr. Jacob within a week.
Embryology
CRMRS laboratories have received Certification from CLIA and Accreditation by the Reproductive Laboratory Program of the College of American Pathologists (CAP). Our laboratories are also certified for human tissue handling by the Federal Drug Administration (FDA). In addition, we are enrolled in proficiency testing programs with the College of American Pathologists.
Procedures done in the Embryology Lab
- Our state of the art IVF laboratory offers treatments including IVF-insemination of oocytes, ICSI (intracytoplasmic sperm injection), PGT-A/PGS (Pre-Implantation Genetic Testing – Aneuploidy or chromosomal abnormalities and/or single gene defect), and cryopreservation of sperm and embryos for future use in fertility treatments or fertility preservation.
- In preparation for the oocyte retrieval, we will complete a checklist. Infectious disease testing, hormone monitoring, follicle tracking, consents for IVF/ICSI/AH/Cryo, injection teaching and IVF education.
- Egg retrieval and culture will take place when the hormone levels, uterine lining, and follicles are at the most optimal level to achieve positive outcome. Eggs are retrieved by the ultrasound guided follicle aspiration while the patient is under light sedation. Eggs will be cultured in the incubator at optimal temperature, pH and humidity levels, for the duration of the in vitro culture. The culture medium is placed in the incubator in preparation of the oocyte retrieval on the day before egg retrieval.
- Oocyte vitrification can be utilized for patients wishing to preserve fertility. Typically this is used when a patient does not have a spouse and wishes to freeze eggs before advancing age, or in most cases prior to chemotherapy or radiation treatment for cancer. One of the advantages to cryopreservation of embryos or oocytes is the frozen embryo transfer and preparation of the uterine lining does not require stimulation drugs and oocyte retrieval. The costs are less and the cycle is less stressful for the couple without the necessity for all of the injections, monitoring visits and blood draws.
- Conventional insemination of oocytes with fresh, washed and activated sperm, will occur several hours after the egg retrieval.
- For ICSI the eggs are denuded (outer cells removed with a mild enzyme) and the presence of the PB (polar body) is used to determine the maturity of the oocytes. If the PB is present the sperm will be injected directly into the cytoplasm of the egg. For those eggs which are not mature at the initial injection time, continued culture and observation for maturity followed by injection of sperm when they have matured may be done. This is considered day 0. The embryologist will notify the couple at the end of the day to update them on the number of eggs that were injected.
Day 1: Fertilization check and continued culture of pre-embryos. The embryologist will notify the couple of the number of eggs that have fertilized. The presence of 2 pronuclei (PN) is a normal fertilization of the egg and the abnormal fertilization may have only 1 PN or 3 PN. This will begin to give us an idea as to whether the embryo transfer will be on day 3 or day 5. We would like to have at least 4 good quality embryos on day 3 to continue culture to day 5.

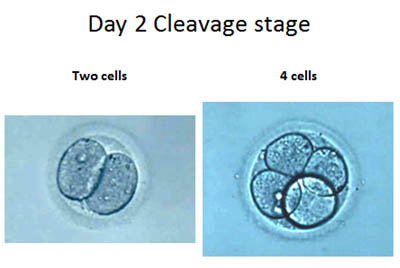
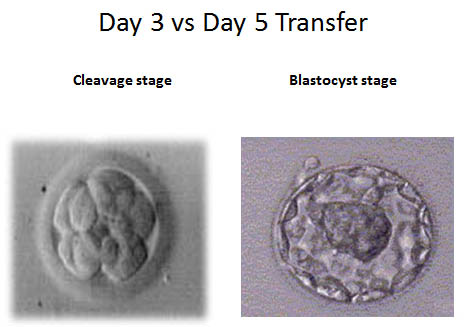
Day 2: Cleavage check. The day after fertilization occurs, the embryo begins to cleave or divide. One cell becomes two and so forth. On day 2 we should expect to see 2-4 cells in the growing embryo. We will note the even size of the cells and the amount of fragmentation. This will give us a better idea as to the quality of the embryos and the decision to have day 3 vs. day 5 ET may be made on day 2. If the quality of the embryos is such that we have a clear decision as to which embryos will be transferred, we may decide to have a day 3 ET. If there are 4 or more good quality embryos and we want to culture to blastocyst for the final decision as to which embryos will be placed back in the uterus, we will continue culture to day 5.
Day 3: Cleavage stage embryos should be at the 6-8 cell stage with minimal fragmentation. Assisted hatching can be done to embryos which have a thick membrane (zonapellucida). This is accomplished by using a mild acid solution and making a small hole in the membrane.
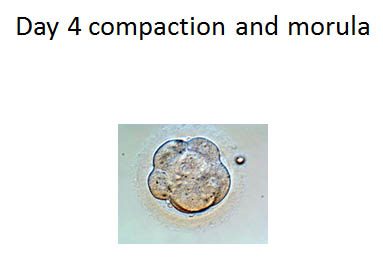
Day 4: Embryos that are cultured to blastocyst will begin compaction and become Morula. The Morula is the precursor to the blastocyst. The cell number is now about 90-100 cells and can’t be counted. We are looking for minimal fragmentation and compaction of the cells with the beginning of a cavity forming. This cavity is the fluid filled area of the embryo.
Day 5: Good quality embryos should be reaching the blastocyst stage. The blastocyst has three important components. The trophectoderm layer of trophoblastcells whichbecomes the placenta. The ICM (inner cell mass) becomes the fetus, and the fluid-filled cavity becomes the amniotic fluid. Embryos are graded at this time and the best quality embryos are selected for embryo transfer to the uterus.
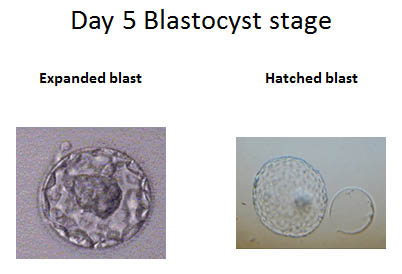
- Hatching embryos may be observed on day 5 or day 6. The embryo must hatch out of the membrane in order to attach to the uterine lining and pregnancy occurs with implantation.
- m. Vitrification of embryos is typically at the 2PN, cleavage stage or blastocyst stage. Vitrification of 2PN embryos is generally done when a fresh embryo transfer is not planned and the embryos are cryopreserved for a future frozen embryo transfer. Blastocyst cryopreservation is typically done after the embryo transfer and remaining embryos that are of a good quality are frozen for future use in a frozen embryo transfer.
- n. The cryo storage bank is generally for embryos and sperm that will be used within the next 3 years. If long term storage is desired, there are several storage banks that are available and may be more cost-effective for the couple
Andrology
Male Factor Infertility plays a significant role in reproductive disorders. Up to 40% of couples may be facing male factor infertility. Additionally, there may be 20% of infertile couples that have a combination of male and female infertility. The infertility specialist must rely on adequately controlled sperm function tests to achieve an accurate diagnosis. The Andrology Laboratory at the Center for Reproductive Medicine & Robotic Surgery offers you and your physician a wide range of specialized sperm testing and sperm processing alternatives…
Complex Semen Analysis
Although the semen analysis is not a test of fertility, it is the most important single indicator of the functional status in the male reproductive tract. Clinical studies of infertile patients have established “limits of adequacy” below which the chance of initiating a pregnancy becomes more difficult. A minimum of two evaluations is recommended to establish a profile of the seminal parameters. In addition to sperm density, morphology, motility and viability, we record volume of the ejaculate, pH, viscosity, and presence of any other micro or macroscopic abnormal findings (Strict Kruger criteria). Abstinence must be between 2 and 7 days. If the specimen is collected at home, it will need to be transported within 1 hour to the laboratory and kept warm in a sterile container. The patient’s name, date of birth, date and time of collection must be labeled on the container.
Sperm Function Tests
In addition, the Center offers a range of specialized sperm function testing for the evaluation of male fertility. These include:
- Sperm Antibodies in Male and Female, which determines the presence of antibodies bound to the sperm membrane (Direct) or the presence of circulating sperm antibodies in the female partner (Indirect)
- Hypo-osmotic swelling, which determines the proportion of sperm that contain intact functional membranes by placing the sperm in a solution which will cause the live sperm to “curl tail” and the non-viable sperm will remain straight tailed.(will hyperlink the HOS test video)
- Sperm Overnight Culture, From which a great deal of valuable information may be obtained ( i.e. we can learn if spermatozoa do not survive well in culture, or if they are contaminated with bacteria). If sperm motility after overnight culture is low we may customize the sperm processing methods to obtain the highest number of sperm with the longest survival time.


Sperm washing and concentration for IUI
We have the ability to make sperm preparations using conventional means. In addition, separation of highly motile spermatozoa can be done using gradient centrifugation, swim-up or a combination of these two. Conventional sperm washing requires about one hour, while gradient centrifugation and swim-up may need up to 3 hours to be conducted. Please consult the office for appointments.
Sperm Cryopreservation and Storage
This may be a necessary step for patients wishing to freeze their sperm before they are subjected to vasectomy or other treatments, such as chemotherapy or radiation, that may impair their ability to produce fertile spermatozoa. On the other hand, couples who have busy schedules which do not allow them to have intercourse around the ovulatory days, may opt to have frozen sperm available for IUI.

Cryo bank
Cryopreservation of human sperm (Sperm Banking) was initially employed as an aid to circumvent certain forms of infertility. More recently banking of human sperm has been employed for a number of different reasons. Although this technique has been utilized in humans for more than four decades in the U.S, the potential expectations for the users are not clear. It is the purpose of this website to give you general information about it and help you make an informed decision if you elect to use sperm banking.
Bear in mind that the present information is only a guide based on estimations obtained from the American Society for Reproductive Medicine (ASRM). This does not constitute a guarantee that you are going to achieve a pregnancy with the cryopreserved semen specimens. Basically you are going to weigh your estimated potential to fertilize and produce a pregnancy against the estimated efficiency of the different existing alternatives to conceive and its costs.

Who needs sperm banking
The most common use of human sperm cryopreservation is when anonymous healthy donors provide semen specimens to inseminate women whose partners cannot provide sperm with fertilizing ability. However, if you are in the group of fertile men who are contemplating a vasectomy, or face the necessity to be treated for cancer (chemotherapy and/or radiation) or any other procedure that might jeopardize testicular function and sperm production, then perhaps you may want to have some of your sperm frozen to be utilized later in case you cannot produce sperm in the future.
Can a single semen specimen be fractionated into several doses?
The standard procedure for freezing semen calls for specimens that have at least 20 million motile spermatozoa after thawing. Therefore, if you have an average or above average sperm quality, then it may be possible to fractionate a semen specimen into several specimens. However, it may be questionable to do so if the sperm quality is below average.

How do I know the quality of my semen specimen?
The semen specimen is evaluated before freezing and after thawing . With the information gathered one can estimate the “Total Number of Normal Motile Spermatozoa” that survived freezing. This information, along with the number of specimens frozen and the kind of solution utilized to freeze the sperm, is given to you or your referring doctor. We also keep a copy for our records.
How many semen specimens should be frozen?
The number of specimens to be cryostored may be different for each patient depending on social and biological factors. Your age, marital status, and number of children that you presently have are some of the social factors to consider. Semen quality, health, and your partner’s fertility status may be among some of the biological factors to keep in mind when deciding the number of semen specimens to have frozen. You should also consider the overall pregnancy rates and cost of the currently available reproductive technologies. Pregnancy rates for intrauterine insemination (IUI) or in-vitro fertilization (IVF) are about 20% and 40-70% respectively. For IUI you may need more than one ejaculate; for IVF a single one may only be necessary. For male factor infertility patients with very low sperm counts there is an additional technology available: Intra-Cytoplasmic Sperm Injection (ICSI). Once you weigh all the factors described above you may have an idea about the number of specimens you want to freeze. Let us suppose that in the best of scenarios you are a healthy male, contemplating a vasectomy, have an average or above sperm quality, have a stable family and children, and you want to have semen frozen just for “peace of mind”, you may want to freeze a single ejaculate. In a different scenario if your sperm quality is below average, you have no children, and have health problems that may impair your ability to produce sperm, you may want to play safe and have more than one specimen frozen.


How is my semen specimen stored?
A semen specimen is stored in sterile plastic vials which are labeled with your name, ID #, and date of storage. The vials are attached to aluminum canes. Each cane can hold up to six vials. They are placed in special tanks that contain liquid nitrogen. The temperature of the liquid nitrogen is -196C.
In the event I move to a different city, can my specimens be transferred?
Yes, you can arrange to have your specimen sent to a facility in liquid nitrogen tanks for storage. Most cities with populations of 100, 000 or above should have one such facility. You will be, of course, responsible for any transportation fees.

Embryo cryopreservation
Embryos that are not selected for transfer in afresh cycle can be frozen to allow a patient to return for a frozen embryo transfer at a later time, with minimal medication, less expense and less stress. This may be an option after a failed IVF cycle, for a sibling of the child from the fresh IVF cycle and for family balancing (gender selection) after PGT-A.
Embryos can be frozen at various periods of development depending on the decision of the patient in consultation with her physician:
- 2PN stage, Day 1, (the morning after the retrieval); this is a pre-embryo or zygote
- Multicellular or cleavage stage (>2 cells) typically day 3 with 6-8 cells and minimal fragmentation;
- Expanded blastocyst stage, typically at day 5 or day 6. Only expanded blastocysts with a good trophectoderm layer (which becomes the placenta) and a clearly defined inner cell mass (which becomes the fetus) should be frozen.
Oocyte cryopreservation
Oocytes are frozen at the day 0 stage after the retrieval. Typically, eggs are frozen at this stage to preserve fertility, prior to chemotherapy or other treatment that may affect the quality of the oocyte and affect a woman’s fertility. A patient may also elect to freeze eggs prior to entering into a permanent relationship and wishing to preserve eggs at her current age. Another reason to freeze oocytes may be an early onset of diminished ovarian reserve. This condition is usually seen in some families where the women undergo premature menopause (less than 40 years of age). In all of these instances, the oocyte is vitrified and will remain at that chronological age until it is thawed, fertilized with sperm, and cultured to embryo and then transfer back into the uterus.
Another common use for egg cryopreservation is to delay family for women who is currently in advanced stage of their education or early stage in their career. These women may freeze their eggs when they are young and years later when they are ready to start a family, they could use their frozen eggs to create an embryo and transfer them back into the uterus.
In addition, at our Center, we offer donor eggs to couple needing eggs. These recipient couple or women in same sex relationship can search donor egg database database and select eggs that are appropriate for them.

Additional Laboratory Services
- Cryo bank for sperm banking, embryo and oocyte preservation; GoFertility also offers donor eggs for in-need couples
- Male infertility (andrology) tests, including sperm function, sperm washing and concentration and semen storage
- IVF of oocytes
- ICSI, or intracytoplasmic sperm injection,
- Pre-implantation genetic testing-aneuploidy (PGT-A)
- Egg retrieval and culture performed at optimal levels for positive outcomes
At GoFertility, we use cutting-edge technology combined with our extensive experience to achieve positive results for our patients in their fertility journey. Dr. Jacob is a world-class surgeon who is one of only a handful of U.S. doctors dual-certified as a high-complexity clinical lab director and OB/GYN. You’re in excellent hands at GoFertility, which was ranked a top-50 fertility clinic in America by Newsweek in 2024. Call or email us today, as we look forward to assisting you!